Introduction
Although newer therapies have become available for treating relapsed and refractory acute myeloid leukemia (RR AML), long-term survival and cure rates remain poor1,2. Newer therapies designed to target mutations or specific proteins may be able to improve current outcomes. Venetoclax is an oral B-cell lymphoma 2 (BCL2) inhibitor that gained FDA approval for use in combination with either azacitidine or decitabine or low-dose cytarabine for newly-diagnosed AML in adults ≥ 75 years. Venetoclax has demonstrated clinical activity in RR AML in retrospective studies1,3,4. The purpose of this study is to evaluate the safety and efficacy of venetoclax with either decitabine or azacitidine compared to alternative therapies in RR AML at a large, academic institution.
Methods
This was a single-center, retrospective cohort study conducted at Northwestern Memorial Hospital and Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois that compared outcomes of patients who received venetoclax with a hypomethylating agent (HMA) to those who received alternative treatment regimens for RR AML. Patients were included if they were ≥18 years old, were diagnosed with either relapsed or refractory AML, had failed one or more lines of therapy, and received a chemotherapeutic agent for relapsed or refractory AML. Patients enrolled in clinical trials were excluded. The study period was from August 1, 2017 to November 30, 2019.
The primary endpoint of this study was the combined rate of complete remission (CR) and complete remission with incomplete hematologic recovery (CRi). The secondary endpoints were overall survival, time to CR/CRi, duration of CR/CRi, percentage of patients who received a hematopoietic stem cell transplant (HSCT) after treatment, and safety outcomes. Safety outcomes evaluated included events that required or prolonged hospitalizations, specifically a documented infection, neutropenia, anemia, thrombocytopenia, and tumor lysis syndrome (TLS).
Results
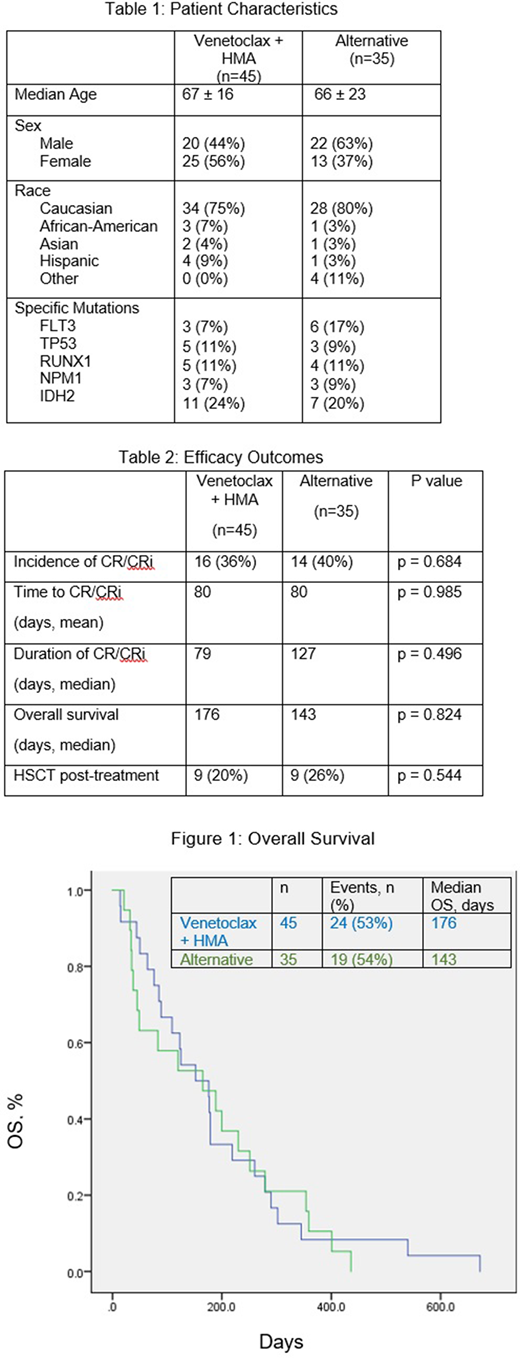
During the study time period, 45 patients received venetoclax + HMA for RR AML and 35 patients received an alternative therapy. Twenty-three patients (51%) in the venetoclax + HMA arm were previously treated with HMA therapy. The most common therapies in the alternate arm were FLAG-IDA, azacitidine monotherapy, and enasidenib monotherapy. Baseline demographics were similar between groups as seen in Table 1. The majority of patients in both arms were classified according to the NCCN risk categories as either intermediate or poor. Patients in the ven + HMA arm received this treatment as a later line of therapy as compared to the line of therapy used in the alternate arm (51% vs 77%, p = 0.095). The rate of CR/CRi was 36% in the ven + HMA arm vs 40% in the alternative arm (p = 0.684) as displayed in Table 2. The median overall survival was 176 days in the ven + HMA arm and 143 days in the alternative therapy arm (p=0.824) as seen in Figure 1. Additionally, the number of patients that underwent HSCT after receiving the treatments evaluated in this study were 20% and 26% (p = 0.544). There were no statistically significant differences between groups in incidences of documented infection (29% in ven + HMA arm vs 54% in alternative therapy arm), neutropenia (58% vs 69%), anemia (36% vs 46%), thrombocytopenia (56% vs 63%), and TLS (18% vs 14%).
In the subgroup analysis in the venetoclax arm, patients who previously received a HMA had a longer overall survival (179 days vs 104 days, p=0.010) and a shorter time to CR/CRi (59 days vs 70 days, p=0.164) than those who did not receive a previous HMA. However, patients with a previous HMA experienced a lower overall incidence of CR/CRi (26% vs 45%, p=0.175) and continued on to a HSCT less often than those who had not received a previous HMA (4% vs 36%, p=0.007).
Conclusions
Overall, rates of CR/CRi, median overall survival, and the number of patients that underwent HSCT after receiving the treatments evaluated in this study were similar between groups. Additionally, incidences of various adverse effects were comparable between the two groups. The outcomes of venetoclax in combination with a hypomethylating agent are comparable to alternative therapies in the relapsed and refractory AML setting.
Altman:ImmunoGen: Research Funding; Amphivena: Research Funding; Genentech: Research Funding; Astellas: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Cancer Expert Now: Consultancy; PeerView: Consultancy; PrIME Oncology: Consultancy; France Foundation: Consultancy; ASH: Consultancy; Novartis: Consultancy; Syros: Consultancy; Janssen: Consultancy; Immune Pharma: Consultancy; Bristol-Myers Squibb: Consultancy; Amgen: Research Funding; Aprea: Research Funding; Glycomimetics: Other: DSMC; Daiichi Sanko: Membership on an entity's Board of Directors or advisory committees; Kura: Membership on an entity's Board of Directors or advisory committees, Research Funding; Biosight: Research Funding; AbbVie: Membership on an entity's Board of Directors or advisory committees, Research Funding; Fujifilm: Research Funding; Kartos: Research Funding; Celgene: Research Funding; Boehringer Ingelheim: Research Funding; Theradex: Membership on an entity's Board of Directors or advisory committees; Agios: Membership on an entity's Board of Directors or advisory committees, Research Funding.
venetoclax for relapsed and refractory AML
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal